A 49 year old woman reports to the Emergency Room and declares that she’s had “some kind of attack.” She seems drowsy and confused, but otherwise stable. Blood is taken as well as an EKG. The woman proceeds to snooze in the ER waiting area for three hours, until it’s time to go pick up her kids, at which point she requests the staff remove the tube from her vein so she can leave and get her children. The nurse asks the woman to sign a “refusal of treatment” form. The woman states that she’s not refusing treatment, she just didn’t get any — she waited three hours, and no one else can pick up the kids. The reception nurse shrugs. The woman signs the “refusal” and then gets in line: two other patients are having needles removed from their arms too. Kid pick-up time is the immovable object that waits for no one.
Upon arriving home, the patient contacts her doctor and asks if she can take a look at the bloodwork and EKG from the ER. The family doctor, being fantastic, makes an appointment 36 hours away. The patient, meanwhile, remembers that mold had been found in her workplace five days prior to her “attack”: some cabinets two doors down from her office apparently fell off the wall, revealing mold. The patient never saw it, she just heard about it, and she knew they were doing “some kind of work” in there to fix it. Could this “attack” have been an allergic reaction to mold spores?
The patient goes over the details of that day: she entered her office at 8am; she met with two students, about an hour apart; she prepped for her classes. Everything seemed fine, aside from some general nasal congestion, which is not unusual. After the second student left it was her lunch break, before teaching, but she wasn’t hungry, so she just closed the office door, took off her shoes, and made a cup of coffee using the kurig machine in her office, and a clean cup that she’d left out on her desk. With her shoes off, she noticed a wet patch on the rug: how did that happen? She didn’t spill water or recall her students spilling water. But, breaktime! So she popped open Duolingo and did three or four questions in French, had maybe two or three sips of coffee, and then began to feel very, very bad.
The attack began as a general feeling of unwellness, like a panic attack, but not a panic attack. Soon it was dominated by extreme nausea and the sense that diarrhea could happen. A massive stomach cramp — what felt like a tightening of the diaphragm, caused agonizing pain and difficulty breathing. She touched her face and realized it was hot and beading with sweat. She crouched on the floor and panted, she took off most of her clothes, trying to cool off. She thought maybe her bra was causing the intense pain in her chest, but it made no difference.
Immediately she imagined how embarassing it would be if her students saw her half naked on the floor having vomited and diarrhea’d all over herself. Embarrassment is a powerful motivator: she didn’t know what was happening to her, but she knew it wasn’t going to happen here, at work, where everyone would see her. What was she thinking? Was it: I want to die at home? Or was it just: HOME.
Getting her clothes back on was an act of tremendous will: quickly she sent a note to all her students that class was canceled and texted her husband that she was sick and going home. you can do this you can do this… She said the words aloud. When she left her office and went down the stairs she saw no one. Stepping outside the building, again, no one: she pictured herself collapsing in the green grass to vomit there and die. But instead she said, you can do this you can do this… and she did the thing that she should not have done: she got behind the wheel of her car and she drove home.
Only after she was driving did she realize she was dizzy. She kept saying you can do this you can do this as she focused on making it through every intersection, on passing cars without colliding. The tightness in her chest got worse. Is this a heart attack? Focus, focus… It was only a three minute drive, and so she made it: she pulled up near her house, parked illegally, and made it indoors, upstairs, into the shower, shedding clothes, her skin felt like it was on fire, her breathing was rapid and loud, all the muscles under her skin were convulsing — had she been poisoned? This is what it would feel like to be poisoned, she thought. But she’d never done anything to piss off Vladimir Putin, so why would she be poisoned?
In the shower she stood then crouched then lay down then stood up in a manic terrorized scramble to find some way to alleviate the horrible feeling that had taken over her body. But no matter what she tried, she couldn’t find relief. Pain, spinning, nausea, panic, muscle contractions, hyperventilation: this was a human body in a state of full blown crisis. She thought of leaving the shower to go downstairs and find a xanax tablet, but moving was hard. She tried to say “you can do this” again, but now she didn’t have breath left for the words.
So she moaned and groaned and forced herself out of the running shower, she hauled her twisting carcass down the stairs and found the xanax, which she placed under her tongue. Then she climbed back up and returned to the shower to blast cold water onto her face, and then hot water onto her clenching diaphragm, and then cold water onto her face again. She remembered there was flonase on the bathroom counter: a steroid that reduces inflammation, maybe it would help? She snorted two squirts in each nostril, then returned to the shower and took deep breaths through the nose.
When her husband arrived at the house, she was naked and soaking wet, lying on her back on the tile bathroom floor, trying to cool her back, neck, and head, because they all felt intolerably hot. Voice shaking between desperate gasps, she said she couldn’t feel her hands or feet — they were tingling and numb. He immediately offered to take her to the emergency room, but she declined, saying she felt too bad to go to the emergency room. Instead she asked him to re-park her car and bring her a loratidine (anti-allergy) tablet. (Sick people cannot be trusted to make good decisions.)
She began feeling slightly better from the nose on out: was the flonase working? More deep breaths through the nose and her breathing slowed down a little. She got up. She dried off. She put on clothes. “Take me to the emergency room,” she (finally!) said.
But once at the ER, there was no doctor available to interpret those test results before the patient, having slept sitting up for three hours, simply had to go home. Once home with her kids, she slept hard all afternoon, then slept through the night, then was tired and drowsy the whole next day. Even the day after that, when she finally got to her regular doctor’s office, she still felt “out of it.”
So what happened?
The EKG taken at the ER 1.5 hours after the attack initiated was normal, which means a heart attack was unlikely. The tingling and numbness in the extremities was almost certainly the simple consequence of hyperventilation.
But the blood taken at the ER showed that all of the patient’s white blood cells were through the roof. The patient had clearly had some kind of massive “stress response” — but to what? The indicator in the bloodwork specifically for an allergic response was strangely normal. Could this possibly have been a panic attack unlike any panic attack this poor lady had ever even fucking heard of?
At the follow up appointment they took more blood, and the reverse was true: the white blood cells had all settled back down except for the category that indicates an allergic response, which was elevated. The doctor prescribed an epi-pen, and referred her to an allergist.
Meanwhile, back in the workplace, other employees were saying that they were experiencing symptoms surrounding the office two doors down from the patient’s office, where the cabinets fell and the mold was revealed.
One person said that when people came to clean off the mold and re-paint, that they had “sanded,” possibly leaving something in the air.
The patient herself recalled that on Monday of that same week (the Monday after the Friday-afternoon cabinet collapose) she’d come in to discover one of her coffee cups, which had been left out dirty, had blossomed thick with round balls of mold like you’d expect if it had been left for weeks. She cleaned it out with soap and water, and didn’t use it again. On the day of the attack, she used another cup that had been sitting out, clean, but in the open air of the room.
Had mold spores been spread through the air and landed in her coffee area? Did she have the attack two sips into a coffee because she was drinking “a concentrated dose” of a toxic mold? Or perhaps the chemicals used to treat the mold affected her in some way? Or did it have something to do with that mysterious wet spot on her carpet, which she stepped into in stocking feet just moments before the attack? What was that, anyway? There was no ceiling leak — could something have been welling up from the floor? The reason she’d laid a rug on her office floor in the first place was because the linoleum tiles were starting to chip up. Maybe that chipping was a sign of a deeper problem in the floor?
Or was this unrelated to the workplace entirely? Was the fact that the attack occurred in her office a mere coincidence? We’re not even sure what caused the attack at this point — we’re just guessing! Just because mold was found two doors down 5 days before, that doesn’t mean someone with no known allergy to mold would end up with this level of health crisis, right? I mean, was this woman even exposed?
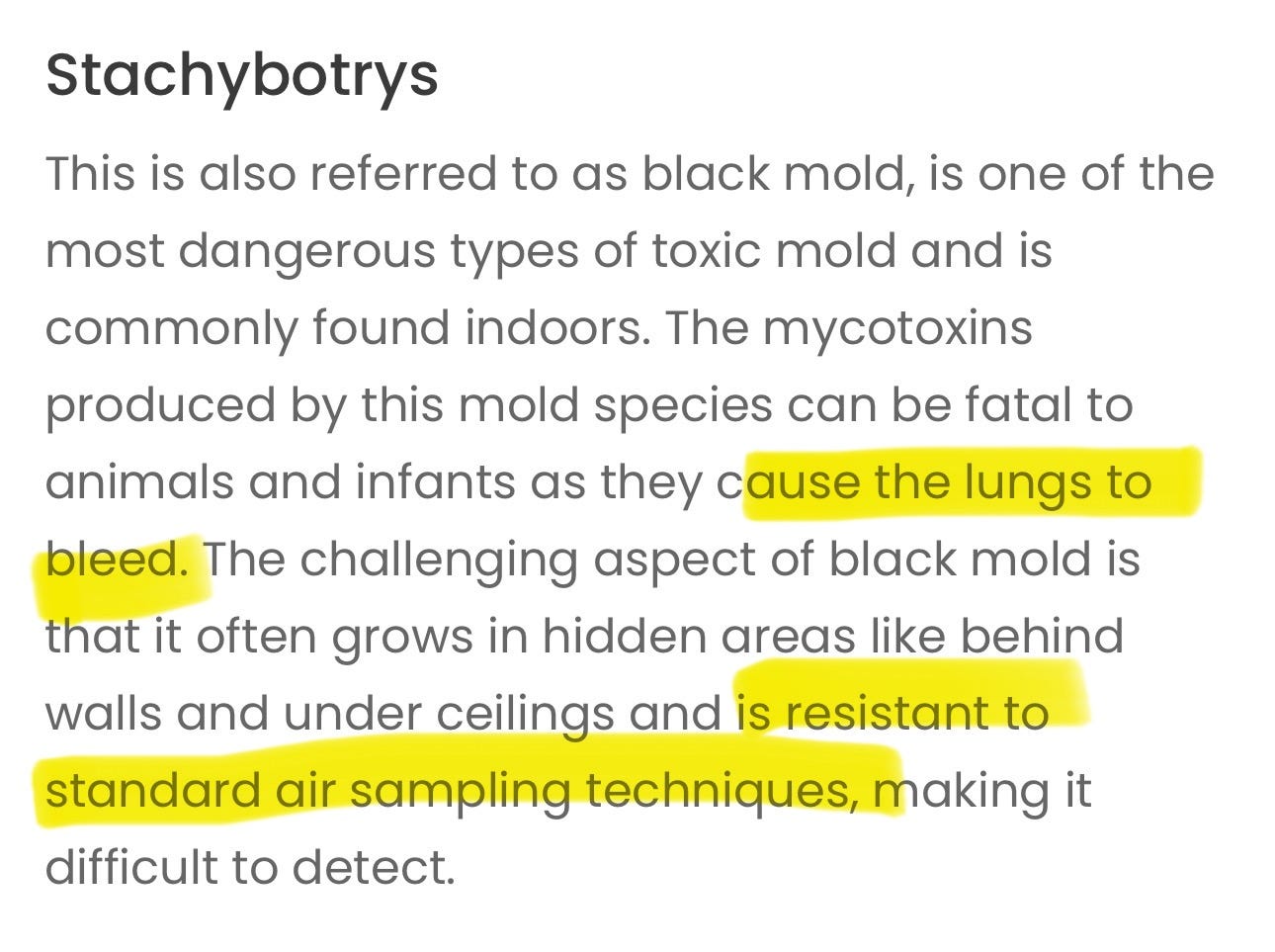
The only way to find out would be by testing the air: flash forward, Stachybotrys spores are found in her office, but at very low levels, just 27 spores per meter cubed. Stachybotrys is nasty stuff: it’s the one people call “toxic mold” or “black mold” or “toxic black mold” — and it’s apparently rarely airborne because its spores are big and sticky, so finding even a little of it in the air is bad news.
The room where the cabinet collapse happened also comes back positive for Stachybotrys, but for half the spore-quantity: just 13 spores per meter cubed. How can the office farther from the source have twice as many spores? Well, there was an attempted clean-up in the room with the cabinets. And maybe conditions on the day of the attack were different from conditions on the day of testing? Or maybe there’s an as-yet-undetected source of spores (more mold) in the patient’s office? Only a thorough examination could tell.
But the fact that the room in the building with the highest toxic spore count, even at just 27 per meter cubed, just happens to be the same room where the employee in residence embarked on a sudden and unplanned near-death experience is a compelling correlation.
How do we solve this medical mystery?
What are the next steps?
What would YOU do?








I had a reaction to stachybotrys that hospitalized me for five days. Stachy can absolutely cause diarrhea and or vomiting. I had a very high fever, rigors and my white cells were so high that they thought I had sepsis. I had cleaned the mold myself and dispersed it into the air. With stachy this is very dangerous. Unfortunately it was in my apartment so I had to dispose of everything ( we hired someone because I could t go back in) Also, when they went in to clean it out there was a layer of geeen and white mold on everything as if it has sat there for months. Turns out through testing it was stachybotrys and aspergillus and penicillin which are very toxic as well and seem to trice together with stachybotrys. If you have any questions at all please feel free to email me at kymwald@ gmail.com
I have two questions: 1) did you look under the carpet? There could be a field of stachybotrys under there.
And, from personal experience, 2) how intense was the pain? The muscle contractions, the nausea, the diarrhea, all of it could have been a stress response to some furious organ in crisis (e.g., a gallbladder passing a gallstone). I would ask for an ultrasound if the mystery deepens.